Breakthrough Injection Could Regrow Knee Cartilage and Prevent Arthritis
Regenerative Knee Injection Rebuilds Cartilage, Fights Arthritis
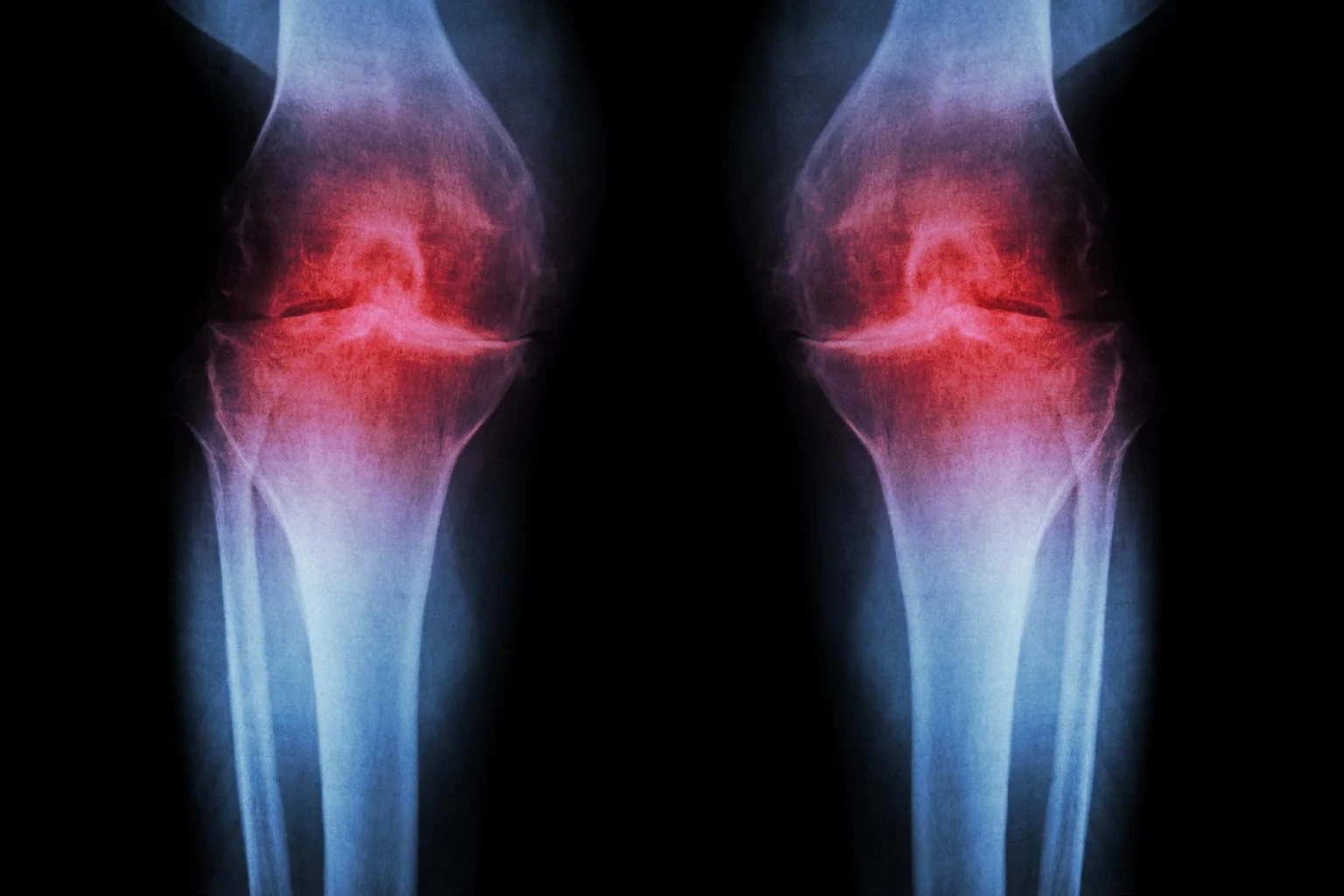
Scientists have unveiled a potentially revolutionary knee injection that stimulates the regeneration of worn-out cartilage and may halt the progression of osteoarthritis — a medical advance that could transform how millions manage joint degeneration and pain.
Osteoarthritis is one of the most common causes of chronic pain and disability worldwide, especially in adults over 50. Until now, treatments have focused primarily on symptom relief rather than restoring the damaged tissue itself. But recent laboratory and preclinical findings suggest that a localized injection targeting the underlying biology of aging cartilage cells could enable the body to rebuild the very tissue that normally fails to regenerate.
This development is generating significant excitement among researchers, clinicians, and patients alike because it tackles a problem that many current therapies can’t: true cartilage loss and joint degradation. By changing how cartilage cells behave, the new treatment may open the door to both preventing and reversing joint disease in humans — including the most debilitating form, knee osteoarthritis.
How the Regenerative Injection Works: Targeting Aging at the Cellular Level
The heart of this breakthrough lies in a protein called 15-PGDH, which scientists classify as a “gerozyme” — a molecule that increases in activity as tissues age and contributes to loss of tissue function. Normally, cartilage in joints has a very limited ability to repair itself, which is why injuries or degenerative changes often become permanent.
In a landmark study led by Stanford Medicine and published in Science, researchers used a small molecule to block the activity of 15-PGDH in aging mice. The result was striking: older animals not only stopped losing cartilage, but they also regrew cartilage that functioned like healthy tissue, and the development of arthritis following joint injury was significantly reduced.
Unlike many other regenerative approaches that depend on stem cells, this therapy works by reprogramming existing cartilage cells (chondrocytes). These cells shift their genetic activity to resemble a more youthful state, enabling them to produce the essential structural components of robust cartilage without needing new cells. This is a fundamentally different mechanism from traditional regenerative methods.
What Research in Human Tissue Shows So Far
One of the most compelling aspects of this discovery is evidence that the biological effect extends beyond animal models. When knee cartilage removed from human patients undergoing joint replacement surgery was treated with the 15-PGDH inhibitor in laboratory conditions, researchers observed lower levels of harmful degradation genes and an increase in genes associated with healthy cartilage formation.

Although these findings come from tissue sample studies and not yet human clinical trials, they strongly suggest the regenerative potential could translate to human biology. Scientists emphasize that turning laboratory success into a safe, effective human therapy will require carefully conducted clinical trials — something the research team hopes to initiate soon, particularly because similar inhibitors are already in Phase 1 trials for muscle decline in aging populations.
Why This Approach is Different Than Current Arthritis Treatments
Most existing strategies for managing osteoarthritis fall into one of two categories:
- Symptom management: Pain relievers, anti-inflammatory drugs, steroid injections, and physical therapy help reduce discomfort but do not rebuild cartilage.
- Surgical intervention: Procedures like joint replacement or cartilage grafting can restore function mechanically, but they involve significant recovery time and cost.
Some advanced therapies, such as mesenchymal stem cell (MSC) injections, have shown promise in inducing cartilage-like tissue growth and reducing symptoms. Studies suggest that MSC injections may foster hyaline-like cartilage repair — closer to natural tissue than scar cartilage — but results have been variable and are still under investigation.
In contrast, the new 15-PGDH targeting technique doesn’t rely on introducing new cells. Instead, it enhances the inherent ability of existing chondrocytes to regenerate, which could eventually make it more reliable and scalable for widespread clinical use if proven safe and effective in humans.
Broader Context: Other Cutting-Edge Cartilage Regeneration Research
The 15-PGDH research is part of a wave of innovative science focused on cartilage repair and osteoarthritis reversal:
- Scientists at Northwestern University have developed a bioactive material that acts like a scaffold, encouraging natural cartilage growth in large animals and mimicking the joint’s microenvironment to support functional tissue recovery.
- A team at the University of Cambridge engineered a responsive material that can deliver anti-inflammatory drugs directly at the site of cartilage breakdown, releasing medication only when inflammation is detected — a smarter drug delivery approach to arthritis.
- In parallel research, innovative hydrogel systems combining anti-inflammatory and cartilage-promoting agents have shown strong results in animal models, accelerating tissue repair while controlling immune responses.
While none of these technologies are approved treatments yet, collectively they paint a promising picture: the era in which clinicians only manage arthritis symptoms might be giving way to an era in which they reverse or prevent joint degeneration.
What This Means for Patients and the Future of Joint Care
If the promising results seen in mice and ex vivo human samples translate into effective human therapies, the implications are enormous:
- Delaying or preventing joint replacement surgery: Millions of patients could maintain natural joint function far longer, reducing healthcare costs and improving quality of life.
- Reducing chronic pain and disability: By addressing the root cause of cartilage loss rather than only mitigating pain, regenerative injections could markedly improve daily comfort and mobility.
- Personalized treatments: Future versions could target specific patient needs — for example, post-injury cartilage loss after sports trauma or age-related wear in older adults.
Researchers caution that clinical trials are essential before this therapy can be recommended for people. Animal and tissue studies are critical steps, but human physiology can respond differently, and safety must be confirmed. Still, experts consider this among the most exciting advances in osteoarthritis research in decades. Stanford News
Conclusion: A New Era in Arthritis Treatment Is Approaching
This emerging cartilage-regenerating therapy represents a significant leap forward in biomedical science. By targeting the biological aging processes that diminish cartilage function, scientists have opened new avenues for treating osteoarthritis — a condition that affects hundreds of millions globally. With ongoing research and forthcoming human trials, what was once thought impossible may soon become a reality: rebuilding damaged knee cartilage and preventing arthritis progression with a regenerative injection.
If confirmed in clinical settings, this science could reshape modern orthopedic care and offer hope to patients long resigned to pain and invasive surgery.
Subscribe to trusted news sites like USnewsSphere.com for continuous updates.