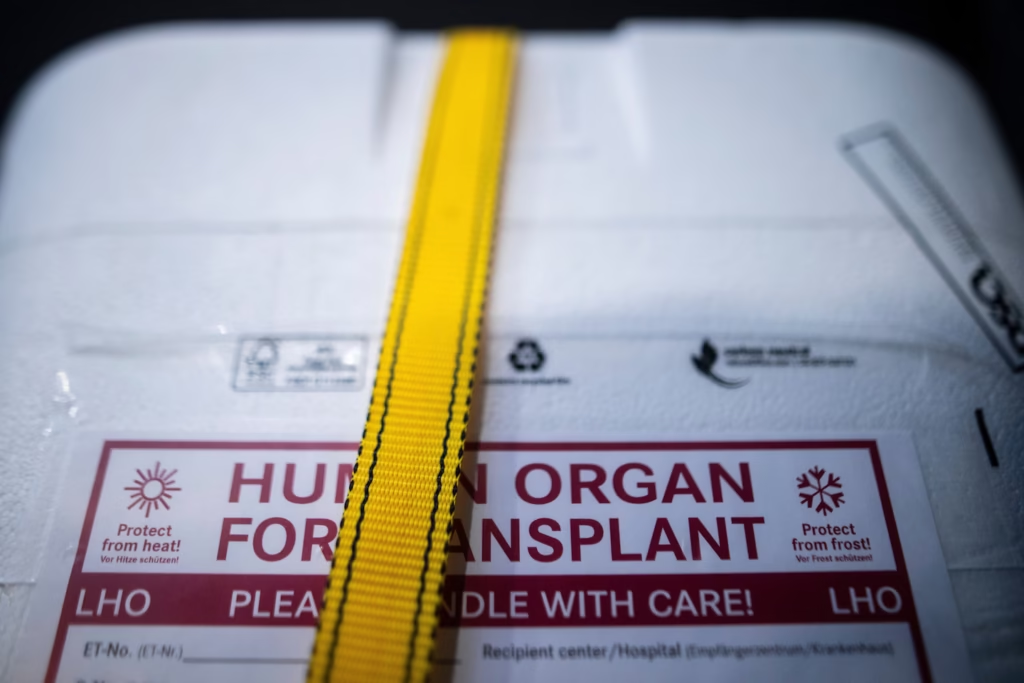
Kentucky man wakes during organ harvesting procedure, sparking urgent federal investigation. In October 2021, Anthony Thomas “TJ” Hoover II—a registered donor declared brain dead after a drug overdose—unexpectedly showed signs of life during preparation for organ retrieval surgery. His family’s account and whistleblower testimonies have since triggered congressional hearings and sweeping reforms across the U.S. organ procurement system.
A terrifying medical near‑miss
TJ Hoover was admitted to Baptist Health Richmond in Berea, Kentucky, following an overdose. Initial evaluations reportedly found no brain activity or reflexes; his family decided to withdraw life support and proceed with organ donation plans. During an “honor walk”—a ceremonial patient procession to the OR—Hoover’s eyes opened and tracked movement, prompting concern from his family despite reassurances that these were reflexes.
Despite these red flags, the procedure progressed. Once in the OR, multiple team members—including surgical preservationist Natasha Miller—observed Hoover moving, thrashing, and shedding tears. Doctors halted the operation after recognizing these signs of consciousness. Miller later claimed she and others were instructed to find replacement personnel to proceed, a directive she resisted. The process eventually stopped, and Hoover was taken home under palliative care. Three years on, he remains alive, suffering from memory, speech, and motor impairments following the ordeal.
From family trauma to national reckoning
The family’s painful testimony and whistleblower accounts—especially from former KODA staff like Nyckoletta Martin—propelled a federal probe led by the Health Resources and Services Administration (HRSA) and the U.S. Department of Health and Human Services (HHS). A critical report identified 73 cases in which neurologically active patients were improperly considered for organ donation; in at least 28 cases, organ recovery may have begun before legal death was declared.
HHS Secretary Robert F. Kennedy Jr. warned of potential decertification for the implicated OPO, Network for Hope—which merged with Kentucky Organ Donor Affiliates (KODA)—if reforms are not implemented swiftly. Lawmakers and medical ethicists across a House Energy and Commerce subcommittee hearing condemned the lapses as “horrifying” and unfit for a system built on public trust.
Systemic flaws in organ procurement protocols
The United States relies on 55 regional OPOs, hospitals, and transplant centers regulated by HRSA and CMS to coordinate organ donation. Most procedures are safe, but they depend on precisely defined death declaration protocols. The system increasingly relies on donation after circulatory death (DCD), raising challenges over brain activity masking clinical death. Investigators found consistent pitfalls, especially in smaller or rural hospitals that may lack experience in donor assessments.
Reforms are underway at the local and national levels
In response, HRSA ordered National and Kentucky OPO reforms:
- Introduction of mandatory checklists for doctors and nurses to identify eligibility and criteria for halting donation processes.
- Creation of anonymous reporting mechanisms for staff concerns.
- Clear new policies empowering any medical staff, family, or donation personnel to pause proceedings if doubt arises.
Network for Hope’s CEO, Barry Massa, acknowledged communication failures—especially amid COVID—and pledged commitment to high safety standards and improvement efforts.
The road ahead: restoring public trust
These revelations have fueled concern that confidence in organ donation may erode. Reports indicate some families have withdrawn from donor registries. Lawmakers stress reforms are urgent—not to stymie donation, but to safeguard donor dignity and prevent similar tragedies.
Experts emphasize redefining the boundaries between hospital care and OPO coordination—while strengthening oversight by HRSA and enforcing transparent incident reporting.
Ethical questions and broader implications
Hoover’s case has stirred national debate over medical ethics in transplantation. Critics argue that economic or procedural pressure may compromise decisions in fragile contexts. While organ donation saves tens of thousands of lives annually, these missteps have highlighted the need to uphold informed consent, strict clinical validation, and ethical accountability. AP News
Conclusion
The case of TJ Hoover in Kentucky has become a pivotal moment for U.S. organ procurement policy—revealing alarming systemic risk, catalyzing reform, and redefining expectations of trust in life‑saving medical systems. With federal regulators mandating new safeguards and practitioners reinforcing protocols, the goal is clear: ensure no donor is declared prematurely, and that every human life is respected, in death as in donation.
Subscribe to trusted news sites like USnewsSphere.com for continuous updates.





